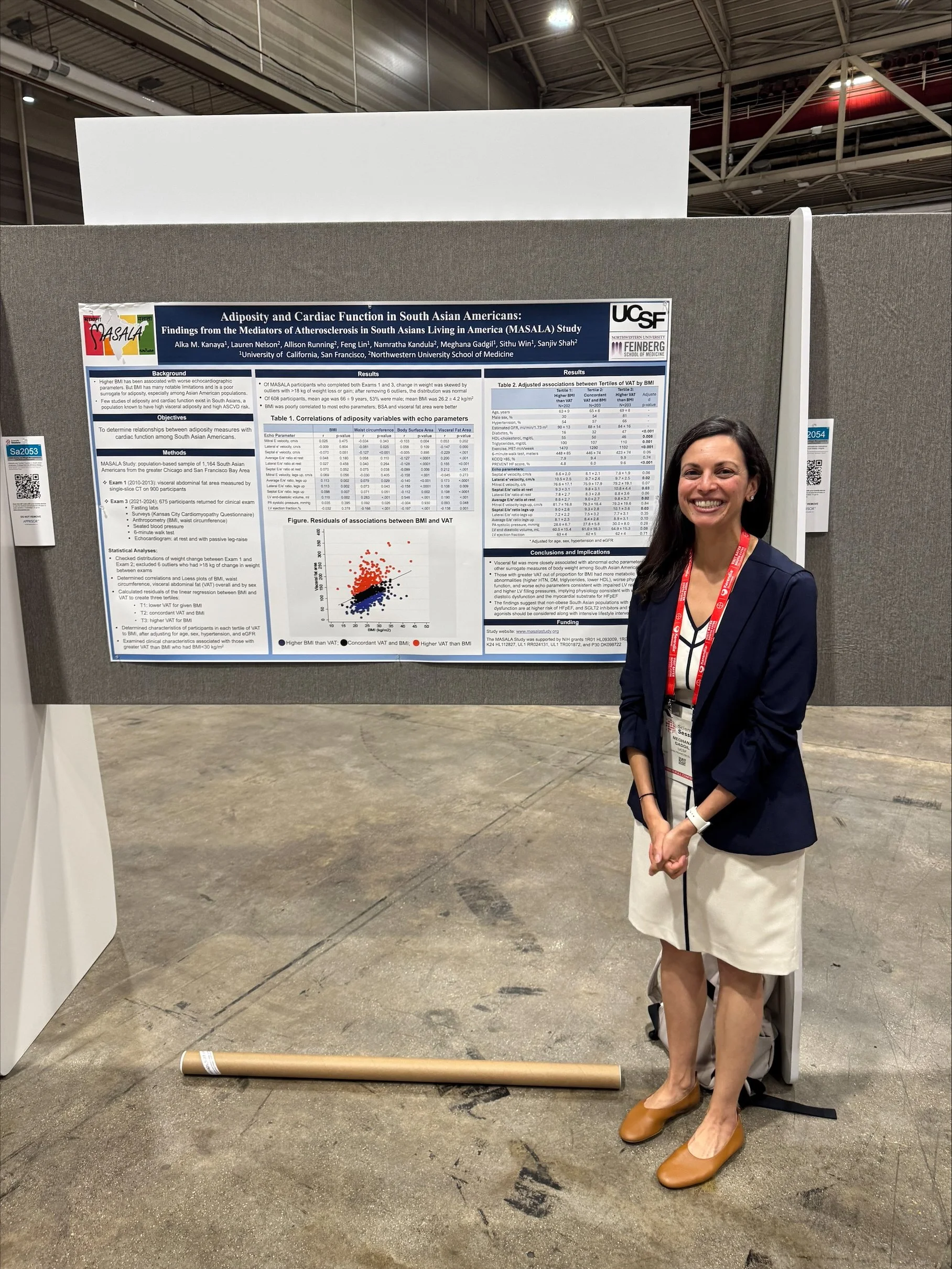
News story: Heart disease risk factors appeared at younger age among South Asian adults in the U.S.
Read the full manuscript here: Prevalence and Trends in Cardiovascular Risk Factors Among Middle‐Aged South Asian Adults Compared With Other Racial and Ethnic Groups in the United States: A Longitudinal Analysis of 2 Cohort Studies